Investing in weight management services

On the 4th March this year, the Government announced £100 million of new funding to help support people in achieving a healthier weight. This is a welcome move given the high prevalence of excess weight in England and the burden it places on individuals, families, social care and the NHS.
Over the last 12 months it has become more apparent than ever that excess weight is a serious matter given the over representation of people living with obesity in intensive care units (ICU) worldwide. Public Health England (PHE)’s analysis last year found that living with obesity increases the risk of severe complications of COVID-19 including hospital admission, ICU admission and death.
The link between excess weight and COVID-19 severity should be no surprise given the well-established relationship with excess weight and a range of chronic diseases, including respiratory health, and the association with reduced life expectancy and quality of life. It has health implications at every stage across the life course, from pregnancy, childhood and adulthood.
For adult weight management services funding is split between the NHS and local authority commissioned services. Funds are also set aside to support services from pregnancy through to those aimed at primary school aged children. Funds for the NHS build on commitments already set out in the NHS Long Term Plan to offer weight management services to people living with obesity and hypertension and/or diabetes. This adds to services already on offer for those at risk of type 2 diabetes through the NHS Diabetes Prevention Programme.
How extra funding for local authorities will be used
Around two thirds of the extra funds for supporting people are ear marked to enhance Tier 2 weight management services (that is, multi-component services: including diet, physical activity and behaviour change components) for adults.
PHE in collaboration with the Local Government Association (LGA) and Association for Directors of Public Health (ADPH) will be supporting the roll out of the Adult Weight Management Services Grant which will distribute £30.5 million among all local authorities in England to commission adult behavioural weight management services in 2021/2022.
The amount each local authority receives will depend on their population size, prevalence of obesity and level of deprivation. The funds can be used to allocate more places on existing weight management services or to buy new services. PHE will support local authorities in setting up new services by developing, in consultation with local authorities, procurement systems that will help authorities to run timely, effective competitions to secure the weight management services that they need.
For children, the Child and Family Weight Management Services Grant will distribute £4.4 million to pilot the expansion of behavioural weight management services and the delivery of extended brief interventions for children identified as being above a healthy weight and their families in 5 to 10 local authorities. Local authorities are invited to apply for funding. As with adults, the level of funding will be allocated based on local need.
For both the adult and child and families grants, conditions will include providing data on weight management service provision at the start and end of the programme, and monthly participant level data. Local authorities will be encouraged to provide equitable access to population groups most in need, including men, people living with obesity from deprived areas and people from Black, Asian and Minority Ethnic groups, and also to enable inclusive services for people with protected characteristics.
What else will PHE do?
PHE and NHS England and NHS Improvement (NHSE&I) are working in partnership to help align NHS and local authority funded services.
Data from services will be used to help make the case for more sustained funding into the future, to learn lessons on service performance and to understand what works best to support good outcomes for all. Evidence on local practice will be collected and knowledge shared.
PHE will work with local authorities and service providers and will develop guidance to support local implementation including on how to ensure that underserved population groups have access to weight management services and how services can be tailored to meet specific needs. Efforts will be made to ensure the voices of people living with obesity are heard and services take a person-centred approach, using non-stigmatising and person-first language.
In partnership with Health Education England, PHE will also support the embedding of Healthy Weight Coaches into primary care and the community by developing training for a broad range of healthcare professionals. The Coaches will engage with people living with overweight or obesity who are interested in improving their health and wellbeing by supporting and motivating them to prioritise weight management and signpost or refer them into weight management services.
PHE will also build the evidence base and identify tools needed to promote healthy lifestyles in the early years to help prevent overweight or obesity concerns in families with young children.
PHE will continue to build on the successes of the Better Health campaign to date by encouraging and supporting people living with overweight or obesity to make positive changes. Campaign activity throughout the next twelve months will promote evidence-based tools and advice including an enhanced NHS 12 Week Weight Loss Plan app to help people develop healthier eating habits, get more active and lose weight.
Where appropriate, PHE will also work in partnership with NHSE&I, local authorities and commercial weight loss providers to help direct people who need additional support to lose weight, into weight management services.
Wider impact of the pandemic on obesity prevalence
Going into the pandemic most adults and a third of children were living with excess weight.
Societal changes associated with the pandemic may have increased the risk of weight gain and made it harder to access weight management services. Over the past year, we have seen changes in the patterns of food purchases and physical activity that may be associated with increased calorie intake and excess weight gain. There have also been changes in societal, economic and psychosocial factors that have been linked to excess weight gain. For instance, rates of unemployment and mental illness have increased during the pandemic.
Therefore, there is incremental change to be achieved by upscaling weight management services as part of place based whole systems approaches to addressing obesity and promoting a healthier weight.
Importance of societal wide actions
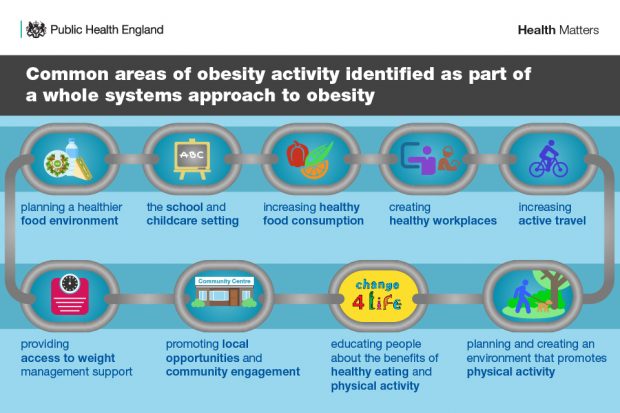
Obesity is a complex public health challenge driven by a mixture of the social, economic, biological and environmental factors that shape our lives and individual behaviours. Due to the multiple factors that impinge on individuals’ choices within the environment where we live, work and play, it is easy to feel the odds are stacked against us when trying to achieve and maintain a healthier weight.
We are living in an obesogenic environment where less healthy options are the default, which encourage weight gain and obesity. For instance, there are many nudges in shops, on TVs, computers and phones that encourage us to buy less healthy food. This is why PHE and ADPH are supportive of Governments commitments to further restrict the advertising and promotion of less healthy food, as well as improving front of pack labelling on pre-packed foods, introducing calorie labelling within out-of-home businesses, including restaurants, cafes and takeaways, and calorie labelling of alcoholic drinks. These are all policy actions designed to empower and support everyone to have access to healthier options.
Given the way the environment can influence people’s behaviour, actions are needed at a local and national level to create a healthier environment to help prevent and treat excess weight. Addressing this is an important part of taking a whole systems approach to tackling obesity and PHE continues to support local areas with this way of working. This includes highlighting some of the positive work already underway in local areas and by supporting Sport England on the local delivery pilot programme and whole systems working to promote physical activity.
Whole systems actions are needed to support healthier options and to stack the odd more in individuals’ favour. That is why PHE will provide further evidence to national and local government to support further actions where they might be needed.
View original article
Contributor: Alison Tedstone

