Moving forward from the prescription medicines review

The first ever evidence review of dependence and withdrawal problems associated with prescription medicines assesses the scale and distribution of the issue and outlines how to ensure people can benefit from the relevant medicines when they are needed, whilst limiting any harms caused by dependence or withdrawal. Find out more in this blog about what this means for patients and what needs to be done.
In response to concerns raised by patients about prescription rates in England and in the context of the opioid crisis in North America, we were asked by the public health minister to review the evidence on dependence and withdrawal problems associated with five classes of prescription medicines in England:
- antidepressants
- opioids (for chronic pain)
- gabapentinoids
- benzodiazepines
- Z-drugs
The review in numbers
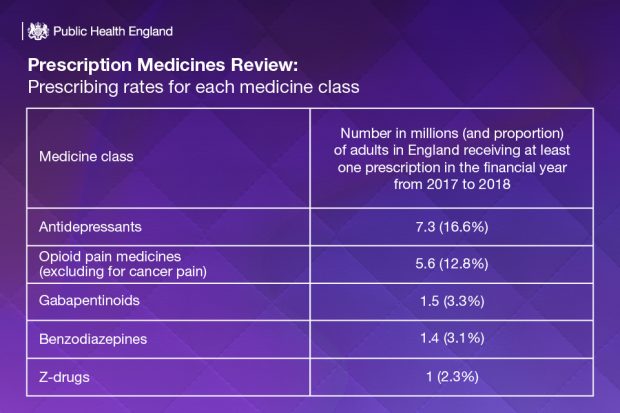
It was found that in 2017-18, one in four adults (11.5 million) were prescribed at least one medicine from these classes. This is broken down by medicine class below:
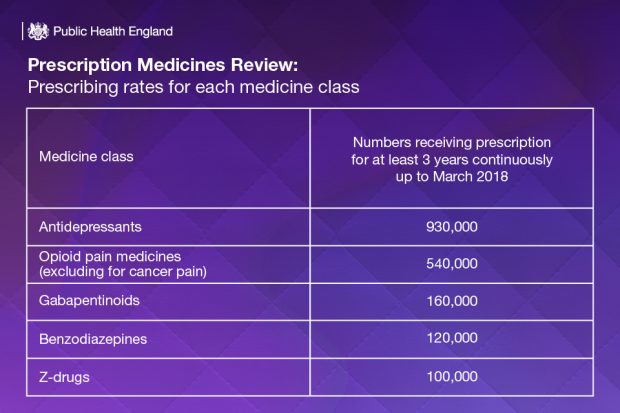
Around half of people who were receiving a prescription in March 2018 had been receiving their prescription continuously for at least 12 months, with higher proportions with longer prescriptions in some of the most deprived areas. When we looked back to 2015, the data reveals that a significant number of people were still receiving their prescription three years later in 2018. This is broken down by medicine class below:
What the review reveals about the current situation in England
There are limitations to what we can say from the available data. We cannot determine the exact number of people dependent on prescription medicines. However, with the amount of people receiving their prescriptions for longer than recommended we can conclude that dependence and withdrawal are likely to be significant issues in England. This is made particularly apparent when considered alongside concerns raised by patients and carers on the harmful side effects and withdrawal symptoms they have experienced that have affected many aspects of their lives.
Guidelines recommend that opioid pain medications and benzodiazepines should be prescribed for short-term treatment of acute conditions. Our review shows that many millions of people are given these medicines well beyond this, risking dependence and requiring careful medical support when they decide to stop.
The situation is different with antidepressants. Many people with depression need to take these medicines for several weeks before they start to help, and many will need to continue taking them long-term. But we must not ignore reports of patients who have experienced severe side-effects from taking antidepressants.
Nobody who has a long-term prescription should stop abruptly – they will need careful medical help to slowly withdraw.
Some patients who have experienced problems associated with withdrawal and dependence have said that their prescriptions were insufficiently reviewed by doctors and that they had trouble finding support. There was also a lack of information on the risks of withdrawal and dependence the medicines can cause, and patients were often not offered other treatment options.
Next steps
In England, our current situation with opioids does not compare to the health crisis in North America – but our review shows that the risk of dependence and withdrawal problems associated with these medicines demand immediate action.
Better support, regular reviews of prescriptions and alternative treatments to medication-alone are all needed to tackle the problem.
We have made recommendations for different areas of the healthcare system to help those experiencing problems and prevent withdrawal problems or dependence. Our recommendations can be found below:

Across the nation, the public need to be made aware of the risks associated with the prescription medicines included in this review and the alternative treatments that are available, including exercise and cognitive behavioural therapy.
Doctors should also be provided with up-to-date guidelines, training and support to ensure effective prevention and treatment approaches are employed when considering medicines that may cause dependence or withdrawal symptoms.
At a local level, prescriptions need to be regularly reviewed and monitored. Publishing accurate data will help local areas identify where they might have problems and provide the push to make appropriate treatment and support available.
At an individual level, doctors need to make sure that they are providing patients with accurate information so that they can make informed decisions about their treatment. This includes information on the risks and benefits of their medication and what other treatment options are available. It is really important that doctors do not inappropriately limit medicines, as this may increase harm, including the risk of suicide, and lead some people to seek medicines from illicit or less-regulated sources. For people experiencing problems with dependence or withdrawal, doctors should be aware of locally available support.
These recommendations are just the beginning of the way forward. The strategic leadership of Clinical Commissioning Groups (CCGs), integrated care systems (ICS) and sustainability and transformation partnerships (STPs) will be vital to implementing our suggestions. We plan to work over the next year with representatives from the organisations that we have made recommendations for, to support their implementation and then establish a working group to take the agenda forwards.
View original article
Contributor: Rosanna O’Connor

