Duncan Selbie’s Friday Message – 17 July 2020

Dear everyone
Risk and investment
The world will never be the same again following the COVID-19 pandemic but this now presents a genuine opportunity to achieve a better balance between risk and investment in the public’s health. PHE is rightly recognised for its science capability, public health expertise and national to local connectivity, but resilience also requires flexibility and ability to adapt to a changing context. No public health agency has entered this pandemic thinking it will look the same afterwards. The public’s health is what matters most and whatever future decisions are to follow, the organising principle will be how we as a nation more effectively close the health gap between the rich and the poor and be better ready in capability and at scale for a future pandemic. Meantime we remain fully focused on fighting the virus.
Protecting seasonal and transient workers
Special thanks to Karen Wright, Director of Public Health for Herefordshire Council, and her Chief Executive Alistair Neill and their teams, for working round the clock this week with our excellent PHE West Midlands team to contain a complex outbreak of COVID-19 in seasonal and transient agricultural workers on a farm in their patch. Careful contact tracing has led the team to subsequently trace more than 100 further agricultural workers in England and Scotland, who have been promptly followed up and offered advice and testing. Exemplary teamwork.
Listening to local people
The critical importance of listening, gaining local knowledge and community engagement was ably demonstrated by Blackburn with Darwen Council this week as they responded decisively to rising rates of COVID-19, notably within their South Asian populations. Listening to local leaders about the way their community lives, works and interacts throughout this pandemic enabled the council to take swift action to protect their residents and hopefully avoid a stricter lockdown. Knowledge, insight, data and partnership working remain the foundation stones to tackling local flare-ups and the council’s approach has empowered everyone to take responsibility, which is a further exemplar of good practice. Listening to people is integral to all public health work, whether we are in a pandemic or not, and the superlative leadership shown in Blackburn with Darwen is a credit to the Director of Public Health Professor Dominic Harrison and the whole council team.
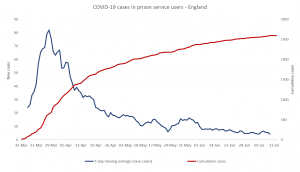
Prisons
A big concern through the pandemic has been the risk of outbreaks in prisons, where people living in close and sometimes crowded conditions can be the perfect breeding ground for COVID-19. PHE has worked closely with HM Prison and Probation Service to protect the prison estate by implementing a population management strategy to enhance social distancing and increase ‘compartmentalisation’ to protect vulnerable inmates and reduce the risk of transmission in other prisons. The evidence so far shows this has been a successful strategy. PHE has led outbreak control teams for each of the 62 reported COVID-19 prison outbreaks, developed surveillance reports to guide public health action and produced guidance on response to incidents and outbreaks. In our capacity as the global lead for the World Health Organization’s Health in Prisons Programme, the PHE team have worked closely with international partners to develop WHO recommendations on the management of COVID-19 in prisons and delivered an international training programme for COVID-19 in prisons as part of the Worldwide Prison Health Research and Engagement Network.
Wider impacts
PHE has published a Wider Impacts of COVID-19 on Health (WICH) tool, which is complementary to our weekly surveillance report. This looks at measures including wellbeing, physical activity, smoking and drinking, as well as how people are travelling and shopping and importantly, the impact on health inequalities. You can see some of the notable findings from the first publication of the tool here.
Seroprevalence
And finally, knowing the extent to which COVID-19 has spread is critical to controlling further spread. As part of this, it is important that we also find people who had mild infections or no symptoms at all, who therefore would have otherwise remained undetected. This can be done by testing blood for the presence of antibodies to the virus and PHE is working with the NHS Blood and Transplant service and NHS laboratories across the country to gather this seroprevalence data. We also have a number of other seroprevalence surveillance programmes underway, including studies testing samples from healthcare workers and school pupils and teachers, and our blog details how this all fits together.
Best wishes
Duncan
You can subscribe to the Friday message newsletter version which goes direct to your inbox here.
View original article
Contributor: Duncan Selbie
