Health Matters: Cold Weather and COVID-19

The latest edition of Health Matters, PHE’s professional resource, focuses on the effects of cold weather on health, looking at how COVID-19 amplifies cold-related risks and actions that can be taken to prevent harm, particularly to the most vulnerable. This blog provides a summary of the full edition’s content.
Cold weather and health
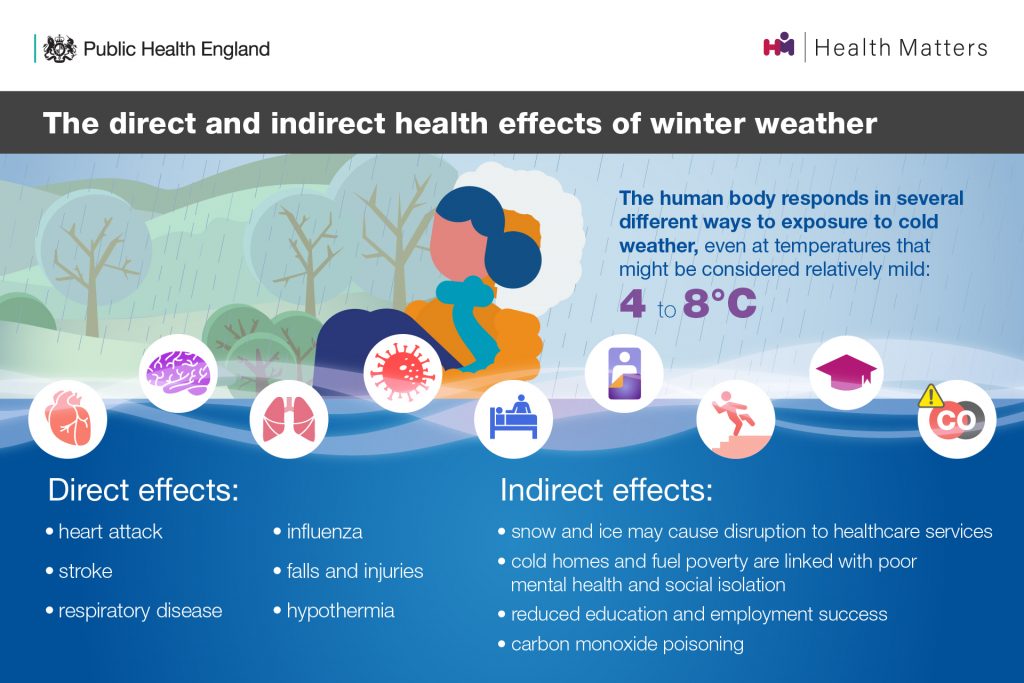
The risk of death increases as temperatures fall, so periods of extremely low temperatures can cause significant harm. However, adverse impacts on health are seen even at outdoor temperatures that might be considered relatively mild (4 to 8°C).
The human body responds in several different ways to exposure to cold weather and it can have both direct and indirect effects on our health.
Cold-related deaths represent the biggest weather-related source of mortality in England. On average, there are approximately 35,000 excess winter deaths (EWDs) each year in England and Wales and there are a number of complex factors that contribute to them.
We may assume that hypothermia is the primary cause of deaths related to cold weather, however heart and lung conditions, as well as dementia and Alzheimer’s are the leading causes. Whilst the greatest impact is seen in older age groups, EWDs do occur across all age groups.
We also know what EWDs represent a significant health inequality, with those experiencing greater deprivation more likely to be affected.
Cold weather and COVID-19
This year, with COVID-19 circulating in England during winter, for the first time, it is critical that plans are in place to address the interacting risks that could arise from the concurrence of cold and COVID-19.
The potential interactions between the two include:
- shared risk factors amongst population sub-groups affected by both cold temperatures and COVID-19
- clinical impacts arising due to concurrence of cold weather and COVID-19
- increased exposure to cold temperatures due to change in patterns of energy use at home, fuel poverty and reduced access to warm public spaces
- reduced access to social and community networks and resources
- change in patterns of health and social care use, access and delivery and health seeking behaviour
Vulnerable people
Certain groups of people are particularly vulnerable to cold weather, including:
- older people, especially those over 65 years old and those who are frail or socially isolated
- People with pre-existing chronic medical conditions
- children under 5
- people with cognitive impairment, mental health conditions or learning difficulties
- people living in deprived circumstances such as experiencing fuel poverty
- people experiencing homelessness or rough sleeping
- pregnant women
Many of these groups are also at greater risk of severe illness from COVID-19, as well as other winter illnesses such as flu. Therefore, it is more important than ever that those most vulnerable are supported this year.
Clinical impacts
We still have much to learn about how COVID-19 infection affects the body, however it is possible that clinical outcomes may be more severe where an individual is exposed to and affected by both COVID-19 and cold weather.
. Longer-term complications of COVID-19 over the months prior to a significant cold weather event may also increase the number of people with vulnerability to low temperatures.
We also know winter is linked to a rise in respiratory infections, but the impact of interactions between COVID-19 and other infections, including the common cold, rhinovirus and bacterial pathogens, is not yet known.
However, there is emerging evidence of poorer outcomes in those who are co-infected with COVID-19 and flu. PHE has recently published new research on the impact of co-infection on disease severity, which you can read about in the Health Matters edition on delivering the flu immunisation programme during the COVID-19 pandemic.
Housing
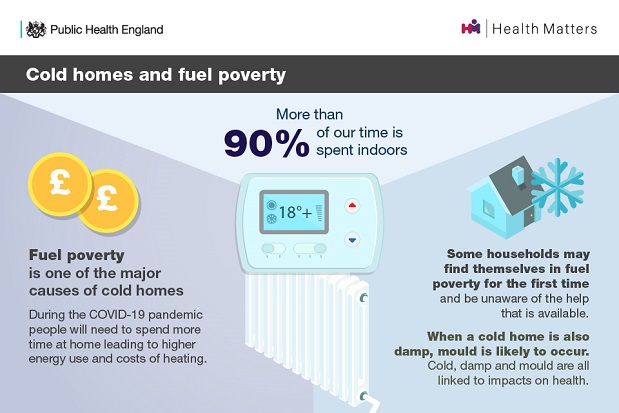
Fuel poverty is one of the major causes of cold homes. When the home is also damp with poor ventilation, mould is likely to occur, and cold, damp and mould all cause a range of health impacts.
During the COVID-19 pandemic, increased numbers of people are spending more time at home than usual, which may lead to a higher demand for energy and an increase in associated costs of heating bills. This winter, new groups of people and households may also be drawn into fuel poverty for the first time and be unaware of the funds and resources available to help with keeping warm.
This edition of Health Matters explores the impact of cold weather and COVID-19 on:
- shared risk factors including olderage
- clinical impacts of COVID-19 and other winter risks
- mental health
- housing and fuel poverty
- homelessness and rough sleeping
- system level risks
Calls to action
This winter, fear of COVID-19 should not prevent action to tackle the risks from cold temperatures and winter weather. It is critical that these preventative actions continue, including identifying and supporting vulnerable people at risk, with necessary adaptations in line with COVID-19 guidance to keep everyone safe.
The Cold Weather Plan for England (CWP) aims to prevent the major avoidable effects on health during periods of cold weather by raising both professional and public awareness. It is a key component of emergency planning and longer term strategic planning, and provides advice for professionals, organisations and individuals to enable them to plan for and respond to cold temperatures.
The CWP is underpinned by the Cold Weather Alert Service, which runs annually from 1 November to 31 March. It comprises 5 levels (Levels 0-4), with each alert level triggering a series of actions from the NHS, local government and public health system, which are detailed in the Plan.
This edition of Health Matters provides calls to action that be used by everyone but also specific actions for:
- health and social care commissioners and Directors of Public Health
- providers of health and social care in all settings
- community and voluntary sector
- national organisations
Visit the Health Matters area of GOV.UK or sign up to receive the latest updates through our e-bulletin. If you found this blog helpful, you can read other Health Matters blogs here.
View original article
Contributor: Owen Landeg
